On July 4, 2025, President Trump signed the One Big Beautiful Bill Act (OBBBA) into law. To partially offset the cost of trillions of dollars in tax cuts, the legislation includes nearly $1 trillion in cuts to Medicaid.
Medicaid generally covers children younger than 18 from families with low and moderate incomes, pregnant women with low and moderate incomes, parents with very low incomes, and individuals with disabilities. In the 40 states that chose to expand Medicaid to adults with low incomes (at or below 138 percent of federal poverty guidelines) under the Affordable Care Act, young adults can qualify based on income alone. Otherwise, they must qualify in other ways, such as being pregnant or disabled.
Extensive research shows Medicaid covers lifesaving care for enrollees. It reduces mortality, can help establish healthy habits, and can lead to higher lifetime earnings. These benefits extend far beyond individuals.
But OBBBA leaves the roughly 3 in 10 young adults ages 18 to 24 insured through Medicaid vulnerable to losing coverage.
How will Medicaid changes reduce young adults’ access to health care?
OBBBA cuts Medicaid spending by changing the program in several ways that affect young adults. Notably, many of the changes target the Medicaid expansion population. Because Medicaid expansion is a key source of health coverage among young adults (PDF), they will likely be disproportionately affected by these changes.
Here are five ways the changes to Medicaid in OBBBA will likely affect young adults in the short and long terms:
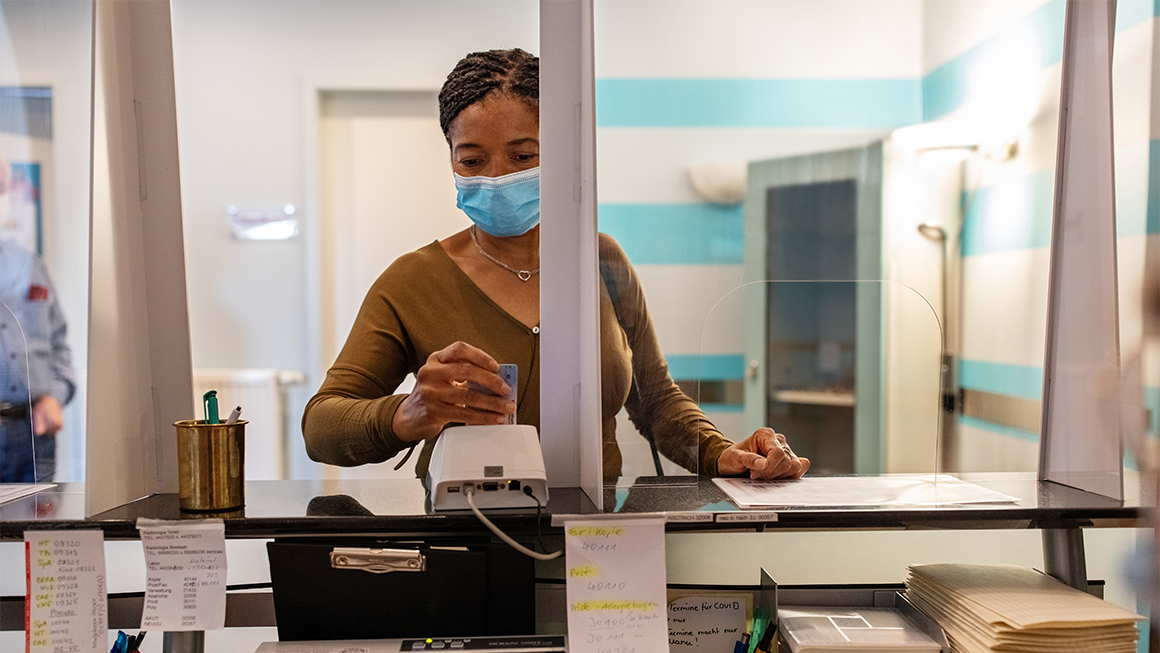
Increasing application and other paperwork requirements could make it difficult for young adults to apply for and maintain Medicaid coverage. Beginning in January 2027, states will be required to conduct eligibility checks for people covered under the Medicaid expansion every 6 months—up from the 12 months currently required. It also reverses course on a rule finalized (PDF) in 2024 designed to make it easier for people to enroll and maintain Medicaid coverage.
Research shows young adults struggle more than older adults to navigate bureaucracy and are also more likely to move than older adults, which could place them at risk of not receiving renewal notifications sent to outdated addresses. Doubling the frequency of eligibility checks for the expansion population will likely hit young adults especially hard.
Work-reporting requirements will likely lead more young adults to lose coverage even if they are working. OBBBA conditions Medicaid expansion coverage on whether beneficiaries work, volunteer, or participate in work-related activities for 80 hours per month or are enrolled in school at least half time, unless they qualify for and receive an exemption based on characteristics such as pregnancy, medical frailty, caring for a disabled family member, or being a parent of a child under 14. New Medicaid expansion applicants must demonstrate they meet this requirement before applying. Enrollees must demonstrate compliance between each eligibility redetermination. OBBBA requires states to implement work requirements starting January 2027. States may request waivers that move up implementation or exemptions that move the implementation deadline to January 2029.
Work requirements will likely put millions at risk of losing coverage. One analysis estimates between 10 and 15 million people, largely from the expansion population, will lose coverage. The number who lose coverage will vary depending on how effectively states use data matching to ease compliance.
Because young adults are more likely to be students and face challenges achieving stable employment, they are particularly vulnerable to losing Medicaid coverage under the new requirements. States are less likely to have data on their work or education that would deem them compliant with stable employment. And the fact that young adults often struggle to navigate bureaucracy will likely compound this challenge.
Higher out-of-pocket costs will threaten young adults’ access to care. OBBBA introduces a new requirement that adults share more of the cost of some types of care if they qualify for Medicaid through the expansion and have incomes over 100 percent of the federal poverty level. The requirement takes effect in fiscal year 2029.
Research shows cost sharing in Medicaid leads to worse access to care and increases financial burden for beneficiaries. This could disproportionately affect young adults, who have historically been more likely than older adults to forgo medical care because of cost.
Medicaid changes will likely reduce young adults’ access to reproductive care and other critical health services. OBBBA withholds one year of Medicaid funding (July 2025–July 2026) from some nonprofit community providers that provide primarily family planning or reproductive services. These are some of the most critical health care needs young adults have. Young women could be disproportionately affected, given that they frequently seek primary preventive services, such as well-woman care, from these providers. This provision is currently being litigated.
Beginning in fiscal year 2027, OBBBA also prohibits states from increasing taxes on health care providers and using this revenue to qualify for federal matching payments. These taxes are an important way states fund their portion of Medicaid costs. Because they will be less able to draw on this revenue source, states are likely to cut provider payments. This will likely reduce the number of providers that accept Medicaid and the amount of services they provide. That would make it harder for all enrollees, including young adults, to access care.
Removing incentives for more states to expand Medicaid will eliminate a key opportunity to increase insurance coverage for young adults. Young adults have the highest uninsurance rateof any age group (about 11 percent) and the lowest rates of employer-provided health insurance.
Starting in January 2026, OBBBA eliminates enhanced federal funding for states that choose to expand Medicaid for the first time. This will likely deter additional states from expanding coverage to adults with low incomes, leaving on the table a key avenue to increase health insurance coverage for young adults.
What can states do to support young adults as they implement OBBBA Medicaid changes?
Taken together, evidence suggests changes to Medicaid in OBBBA will likely create new hurdles for young adults as they work to achieve self-sufficiency.
As states consider how they will implement OBBBA’s changes, they should prioritize access to coverage for as many of the young adults who rely on Medicaid as possible and take steps to mitigate some of the challenges young adults could experience.
For example, to mitigate hurdles young adults face in documenting their compliance with work requirements, states could ensure Medicaid administrators have access to data on school enrollment and develop user-friendly ways to report unstable work, such as allowing people to easily upload documents from a mobile phone. These and other improvements (PDF) to state data and reporting infrastructure may be an effective area to focus implementation resources to support health care access for young adults.
Let’s build a future where everyone, everywhere has the opportunity and power to thrive
Urban is more determined than ever to partner with changemakers to unlock opportunities that give people across the country a fair shot at reaching their fullest potential. Invest in Urban to power this type of work.