
Summer mosquito season may be over, but the threat of Zika virus definitely isn’t. That’s because Zika isn’t strictly a mosquito-borne virus; it can also spread from person to person via sexual contact—and, according to a new Urban Institute study, an alarming number of women of reproductive age don’t know that.
The latest round of the Health Policy Center’s Survey of Family Planning and Women’s Lives found that although the vast majority of women ages 18 to 44 know that Zika can be transmitted by mosquitoes, less than half know that the virus can be transmitted through sexual intercourse.
Who is at risk?
This knowledge gap is cause for concern, since the health risks associated with Zika are significantly higher for women of reproductive age. Though the virus typically causes cold-like symptoms or no symptoms at all in adults, it can lead to serious complications for pregnant women. Zika has been proven to cause microcephaly and other brain defects in infants, and it has been linked to stillbirth, miscarriage, and other birth defects.
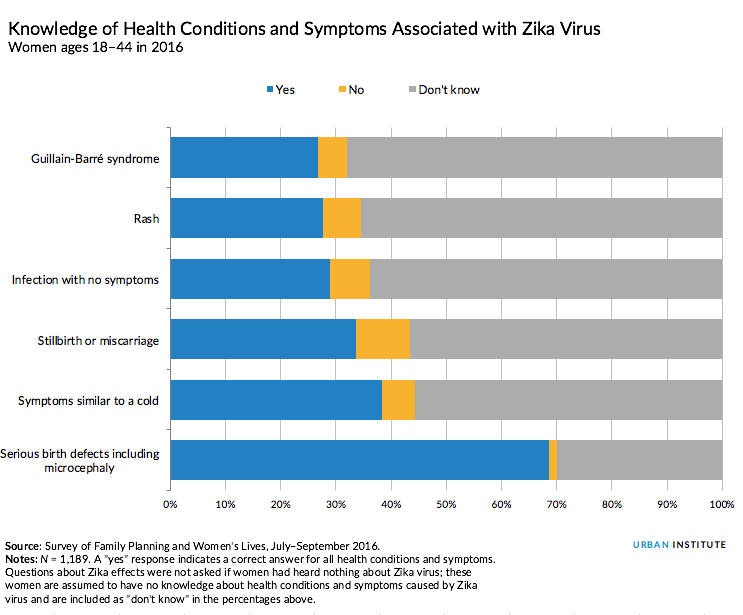
But few women are aware of health effects other than microcephaly. Only 28.8 percent of women of reproductive age know that Zika can cause infection with no symptoms. In fact, four out of five people infected with Zika show no symptoms, so sexually active women could be putting themselves at risk without knowing it. Of the 4,016 people infected with Zika virus in the United States as of October 19, 32 cases have been confirmed to be sexually transmitted.
More than half of women reported taking action because of concerns about Zika, but their preventive behaviors tended to address mosquito-borne transmission. Less than 20 percent reported that Zika concerns made them more likely to use condoms or birth control.
“Women traditionally think about barrier methods as protection against STDs (sexually transmitted diseases) when they’re in nonmonogamous relationships—not when they’re in a committed relationship, or if their partner has been home from a Zika-affected area with no symptoms for weeks,” says Emily Johnston, one of the study’s authors.
What role do health care providers play?
Less than 6 percent of women of reproductive age have talked to a health care provider about Zika virus, according to survey results. Even among women who are pregnant or want to become pregnant—the group at highest risk for Zika complications—only 12 percent reported having the Zika talk.
The lack of communication between women and their doctors isn’t surprising, given the continuing deficiencies in access to health care (not to mention the stigma historically attached to discussions of sexual health).
Though women of all backgrounds missed key facts about Zika’s transmission and health effects, knowledge gaps were most common among women who were younger, lower income, and less educated. Many of these women also lack consistent health insurance coverage. For these vulnerable groups, expanding access to health care could be an important defense against Zika.
“Conversations with health care providers present an opportunity to educate women about Zika virus, but to be successful, women need to first have access to care, such as well-woman visits and reproductive health services,” Johnston says.
What’s next?
There’s still a lot we don’t know about Zika, and official recommendations for its prevention and control are bound to change. For providers and public health officials, that means taking an active role in keeping patients informed and prepared.
On September 28, Congress approved $1.1 billion in new funding to combat Zika. Much of the appropriation is already earmarked for mosquito abatement, vaccine development, diagnostic improvements, and intensive studies of the virus’s health effects.
But new research offers powerful evidence that public outreach and education, specifically for women of reproductive age, should also be a centerpiece of the US Zika response.
Tune in and subscribe today.
The Urban Institute podcast, Evidence in Action, inspires changemakers to lead with evidence and act with equity. Cohosted by Urban President Sarah Rosen Wartell and Executive Vice President Kimberlyn Leary, every episode features in-depth discussions with experts and leaders on topics ranging from how to advance equity, to designing innovative solutions that achieve community impact, to what it means to practice evidence-based leadership.